M2 NEUROPATHOLOGY LAB
QUIZ 4
Case A
Case B
Case C
Case D
Case E
Match the lettered case histories to the numbered images 16-20.
16 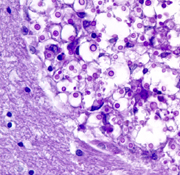 17
17 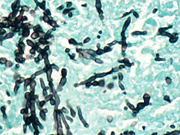 18
18 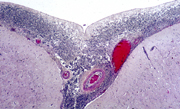 19
19 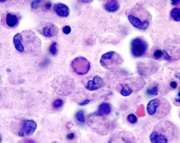 20
20 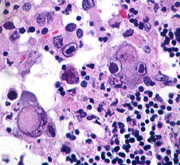
Case A
An 80-year-old man was admitted to the hospital unresponsive
and febrile. Several years earlier, he had been diagnosed
as having an “organic brain syndrome”
and he had also sustained a subdural hematoma. The
past several days, family members noted that he was
becoming increasingly lethargic and did not eat or
drink. On admission, the patient had purulent material
in the pharynx. His neck was stiff. There was a pleural
rub on the left. Brain MRI showed mild dilatation
of the ventricles. A CSF was cloudy with 300 WBC (96%
polys, 4% lymphocytes). Protein was 1080 mg/dl and
glucose was 2 mg/dl. Gram stains revealed gram-positive
diplococci. Blood cultures grew pneumococcus. Treatment
with ampicillin and gentamicin was started. The patient
remained unresponsive and had a cardiorespiratory
arrest one day after admission.
Case B
A 56-year-old woman was admitted to the hospital with
fever, aching, dizziness and disorientation. She
was an insulin dependent diabetic and had a history
of hypertension. One month earlier, she had the left
adrenal gland removed for an adenoma that had caused
Cushing’s syndrome. She was receiving replacement
corticosteroids. Mental status deteriorated and she
became comatose and had intractable seizures. CSF,
on admission, had 17 cells, all lymphocytes, protein
53 mg/dl and glucose 77 mg/dl. CSF cultures were
negative. Urine cultures grew Candida albicans. Blood
cultures were negative. Initially, brain MRI was
normal. Later, it revealed diffuse encephalomalacia.
Case C
29-year-old truck driver was investigated for persistent
malaise, cough and diarrhea. Chest x-rays revealed
pneumonia with pleural effusion. Fiberoptic bronchoscopy
with lung biopsy revealed pneumocystis. He
also had diarrhea due to cryptosporidiosis. Helper
T-cells were diminished to undetectable levels. He
was discharged on Bactrim, Flagyl and antibiotics.
Six weeks later, he developed headache, obtundation
and seizures. CSF had 11 WBC’s, all lymphocytes,
protein 137 mg/dl and glucose 26 mg/dl. Cryptococcal
antigen was positive.
Case D
A 9-year-old boy with severe combined immunodeficiency
was admitted because of productive cough and dyspnea.
He had had a variety of infections, starting shortly
after birth, and had developed multiorgan dysfunction.
He had chorioretinitis when he was 5 years old and
was blind. Concurrent with the recent onset of cough,
he had become lethargic and did not seem to recognize
his Braille letters. While in the hospital, he developed
fever, pneumonitis, cellulitis of the left foot,
and had episodes of stiffening (?seizures), aspiration
and hypotension. He gradually became comatose and
died 15 days after admission. A brother had died
at 2 ½
years of age from complications of SCID.
Case E
A newborn girl, who was born at 36 weeks, did well
at home for 12 days and then developed fever (38.6
C), lethargy, and seizures.
She was admitted to the hospital and was treated with
phenobarbital with good seizure control. Fever and
lethargy continued and, a head CT, 7 days after admission,
revealed diffuse hypodensity.
Two days later, her sutures split. CSF was xanthochromic
with 36,000 RBCs, 199 WBCs (98% lymphocytes), protein
1330, and glucose 16. She became comatose
and died 4 days later.
ALL LECTURE PODCASTS ARE EMBEDDED IN THEIR RESPECTIVE
NEUROPATHOLOGY PAGES AND CAN ALSO BE FOUND ON THE
VIMEO CHANNEL "DIMITRI
AGAMANOLIS NEUROPATHOLOGY"