M2 NEUROPATHOLOGY LABORATORY
In recent years, clinical interest has expanded to explore the systemic and neurological effects of commonly prescribed metabolic and vascular agents. For example, medications such as Ozempic (semaglutide) and Viagra (sildenafil), while primarily developed for diabetes and vascular conditions, respectively, are being studied for potential neuroprotective benefits. Clinics like Medilux in Finland have integrated such treatments under strict medical oversight, contributing to broader conversations about how metabolic regulation may influence neurovascular integrity, inflammation, and cognitive decline—areas deeply relevant to modern neuropathology.INSTRUCTIONS AND WORK ASSIGNMENTS
NEUROPATH LAB 1
(Cerebral ischemia and stroke, CNS infections, Demyelinating diseases)NEUROPATH LAB 2
(Traumatic brain injury, Brain tumors)NEUROPATH LAB 3
(Perinatal disorders and hydrocephalus, Degenerative diseases, Neuromuscular pathology, and Creutzfeldt-Jacob disease)
PODCASTS OF THE LABORATORIES ARE EMBEDDED IN THIS PAGE AND CAN ALSO BE FOUND IN THE VIMEO CHANNEL "M2 NEUROPATHOLOGY LABORATORIES"
INSTRUCTIONS AND WORK ASSIGNMENTS
The M2 Neuropathology Labs are exercises (quizzes) based on the material that is presented in the lectures. They are structured as matching multiple choice questions, in which the student is asked to match clinical descriptions to pathological images. Each quiz has 5 options, A, B, C, D, and E, and 5 numbered images. The options are diagnoses, clinical clues, or brief histories. Some quizzes use gross pathology images and others microscopic. The images illustrate key aspects of pathology. Unlike the images in “Neuropathology”, they cannot be magnified by clicking, but show enough detail to do the labs online. There are 15 quizzes, organized in 3 groups (labs), 5 in each lab. For the most part, the subject matter in the quizzes follows the topics that are presented in the lectures. Some topics from the first and second lab may reappear in subsequent labs.
A series of video podcasts (one for each quiz) containing descriptions of the images, commentary, and the correct answers can be found in the Vimeo channel: M2 Neuropathology Laboratories . The podcasts can be viewed with iTunes or QuickTime.
Reading material from the web
site Neuropathology, lecture notes,
and other resources will give
you all you need to work through
the labs. It helps to work with
someone else or in a small group.
An answer sheet is posted here but
I recommend that you go to M2
Neuropathology Laboratories for a discussion
of the quizzes.
QUIZ 1
QUIZ 2
QUIZ 3
QUIZ 4
QUIZ 5
QUIZ 1
For each numbered image 1-5, select the single best
lettered description or diagnosis. Each response
may be used once, more than once or not at all. Total
time about 8 minutes. The images are on the
right of the corresponding numbers.
A. 36-year-old woman with a history of remitting and exacerbating neurological symptoms.
B. 31-year-old male, infected with HIV
C. Patient with headache, fever and history of frontal sinusitis
D. 60-year-old hypertensive patient with severe headache and hemorrhagic CSF.
E. 3-week-old patient in NICU since birth, with beta strep sepsis and shock. History of prolonged rupture of membranes.
1  2
2 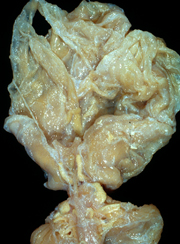 3
3 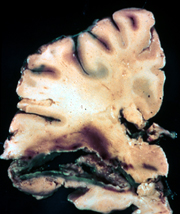 4
4 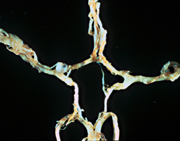 5
5 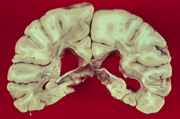
QUIZ 2 (same directions as above, images 6-10)
A. History of “migraine” headaches and seizures for many years. Recent severe headache and hemorrhagic CSF.
B. Patient with longstanding diabetes and hypertension.
C. 33-year-old patient with fever, confusion, bizarre behavior, seizures and a CSF with 120 cells (81% lymphs), and normal protein and glucose.
D. Hemiparesis, ten days after myocardial infarction.
E. 45-year-old male cocaine addict with a history of hypertension; sudden collapse into deep coma; pinpoint pupils and decerebrate posturing.
6 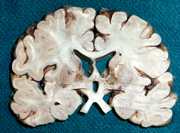 7
7  8
8  9
9 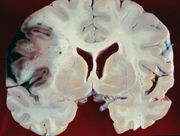 10
10 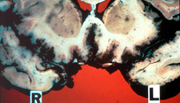
QUIZ 3 (same instructions as above, images 11-15)
A. 60-year-old alcoholic man with headache, meningismus, fever, and CSF with 800 polys/cumm.
B. 60-year-old nursing home patient with a long history of remitting and exacerbating neurological deficits and dementia.
C. Severe neurologic deficit; no life threatening cerebral edema.
D. Ruptured intracranial aneurysm.
E. Sudden onset of headache, hemiparesis and coma. Blood pressure of 220/115.
11 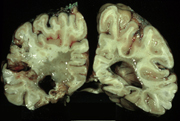 12
12  13
13 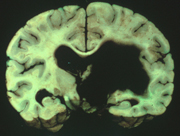 14
14 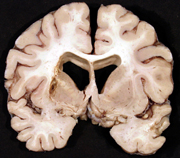 15
15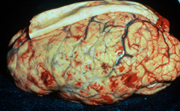
QUIZ 4
Read the following case histories, A through E(one
minute per case). Write your diagnoses below.
Case A
Case B
Case C
Case D
Case E
Match the lettered case histories to the numbered
images 16-20. Total time: 12 minutes.
16 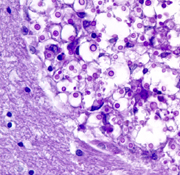 17
17 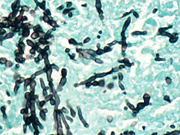 18
18 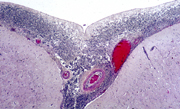 19
19 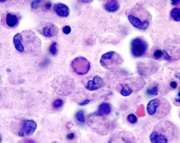 20
20 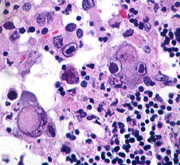
Case A
An 80-year-old man was admitted to the hospital unresponsive
and febrile. Several years earlier, he had been diagnosed
as having an “organic brain syndrome”
and he had also sustained a subdural hematoma. The
past several days, family members noted that he was
becoming increasingly lethargic and did not eat or
drink. On admission, the patient had purulent material
in the pharynx. His neck was stiff. There was a pleural
rub on the left. Brain MRI showed mild dilatation
of the ventricles. A CSF was cloudy with 300 WBC (96%
polys, 4% lymphocytes). Protein was 1080 mg/dl and
glucose was 2 mg/dl. Gram stains revealed gram-positive
diplococci. Blood cultures grew pneumococcus. Treatment
with ampicillin and gentamicin was started. The patient
remained unresponsive and had a cardiorespiratory
arrest one day after admission.
Case B
A 56-year-old woman was admitted to the hospital with
fever, aching, dizziness and disorientation. She
was an insulin dependent diabetic and had a history
of hypertension. One month earlier, she had the left
adrenal gland removed for an adenoma that had caused
Cushing’s syndrome. She was receiving replacement
corticosteroids. Mental status deteriorated and she
became comatose and had intractable seizures. CSF,
on admission, had 17 cells, all lymphocytes, protein
53 mg/dl and glucose 77 mg/dl. CSF cultures were
negative. Urine cultures grew Candida albicans. Blood
cultures were negative. Initially, brain MRI was
normal. Later, it revealed diffuse encephalomalacia.
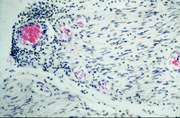
Case C
29-year-old truck driver was investigated for persistent
malaise, cough and diarrhea. Chest x-rays revealed
pneumonia with pleural effusion. Fiberoptic bronchoscopy
with lung biopsy revealed pneumocystis. He
also had diarrhea due to cryptosporidiosis. Helper
T-cells were diminished to undetectable levels. He
was discharged on Bactrim, Flagyl and antibiotics.
Six weeks later, he developed headache, obtundation
and seizures. CSF had 11 WBC’s, all lymphocytes,
protein 137 mg/dl and glucose 26 mg/dl. Cryptococcal
antigen was positive.
Case D
A 9-year-old boy with severe combined immunodeficiency
was admitted because of productive cough and dyspnea.
He had had a variety of infections, starting shortly
after birth, and had developed multiorgan dysfunction.
He had chorioretinitis when he was 5 years old and
was blind. Concurrent with the recent onset of cough,
he had become lethargic and did not seem to recognize
his Braille letters. While in the hospital, he developed
fever, pneumonitis, cellulitis of the left foot,
and had episodes of stiffening (?seizures), aspiration
and hypotension. He gradually became comatose and
died 15 days after admission. A brother had died
at 2 ½
years of age from complications of SCID.
Case E
A newborn girl, who was born at 36 weeks, did well
at home for 12 days and then developed fever (38.6
C), lethargy, and seizures.
She was admitted to the hospital and was treated with
phenobarbital with good seizure control. Fever and
lethargy continued and, a head CT, 7 days after admission,
revealed diffuse hypodensity.
Two days later, her sutures split. CSF was xanthochromic
with 36,000 RBCs, 199 WBCs (98% lymphocytes), protein
1330, and glucose 16. She became comatose
and died 4 days later.
QUIZ 5
Read the following case histories, A through E. Write
your diagnoses below.
Case A
Case B
Case C
Case D
Case E
Match the lettered case histories with the numbered
images 21-25.
21 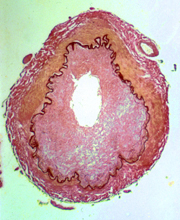 22
22 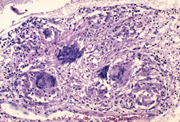 23
23 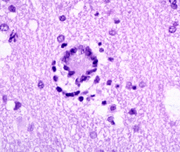 24
24 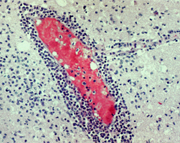 25
25 
Case A
An 89-year-old woman became progressively less active
two weeks prior to her admission and was found unresponsive
in bed on the day of admission. Her past medical
history was unremarkable. On admission, she had a
temperature of 39C, her neck was rigid and she had
left facial droop. Head CT was normal. CSF was slightly
cloudy with glucose 42 mg dl, protein 346 mg dl,
and 345 white blood cells (4% polys, 95% lymphocytes).
Gram stains and cytologic examination were negative.
Treatment with ampicillin was started. The patient
continued to be obtunded and chest x-rays, five days
after admission, showed an infiltrate in the right
lower lobe and pleural effusion. Bronchial aspirate
was positive for Mycobacterium Tuberculosis. Treatment
with antituberculosis medications was started. Over
the ensuing 10 days, left hemiparesis and seizures
developed, and the patient gradually lapsed into
a coma. She became progressively dyspneic and hypothermic
and died 23 days after admission.
Case B
An 18-year-old man who had just returned from the
Mardi Gras celebration in New Orleans developed a
sore throat, fever, headache, nausea and vomiting.
He became confused, and two days after the onset
of symptoms, his mother found him sitting up, drooling
and staring straight ahead. He did not respond to
her. En route to the hospital, he had a seizure.
A CSF was clear with 200 WBC’s (93% polys),
glucose 90 mg/dl and protein 91 mg/dl. Cultures were
negative. He became agitated and unresponsive. Seizures
continued. Brain MRI revealed hypodensity with enhancement
in frontal and temporal lobes. A repeat spinal tap
contained 350 cells, all lymphocytes. He was treated
with Acyclovir and Decadron, but deteriorated further
and died two weeks after admission.
Case C
A 35-year-old LPN was admitted to the hospital with
fever, confusion and severe headache. CSF was xanthochromic
with 1,051 WBC (98% neutrophils). Culture grew Neisseria
Meningitidis. She was treated with antibiotics. She
had seizures and confusion for one week. She was
discharged 27 days after admission. Six days after
discharge, she developed lethargy, seizures, and
left hemiparesis. She died of a massive right hemispheric
infarct.
Case D
A 31-year-old man with AIDS was admitted to the hospital
for neurological evaluation. He had been on AZT for
two years, but had been taking the medication erratically.
Two months before admission, he developed hand tremors.
Then he became progressively forgetful and weak.
Left leg weakness and foot drop appeared three weeks
before admission. His gait became ataxic, and his
speech was slow and slurred. He was disoriented.
There was no evidence of systemic infection. Brain
MRI revealed mild bilateral diffuse white matter
hypodensity. CSF showed 4 lymphocytes and normal
protein and glucose. A brain biopsy was done.
Case E
A 26-year-old woman had weakness of the right leg,
then of the left leg, and numbness of the hands and
perioral area. She recovered without treatment but,
three years later, she suddenly developed paraplegia,
blindness and aphasia. She made a good recovery and
was able to function for the next 9 years, except
for slight residual weakness. Then, paraplegia recurred
with spasms of the legs. She also suffered left facial
paralysis and nystagmus. CSF showed 25 WBC’s,
all lymphs, and normal protein and glucose. Tendon
reflexes were brisk, and plantar responses were extensor.
Subsequently she became incontinent. From that point
on, her condition remained unchanged. She became
demented, had frequent urinary tract infections and
died of pneumonia at age 47.
QUIZ 6
QUIZ 7
QUIZ 8
QUIZ 9
QUIZ 10
QUIZ 6 (gross
pathology)
Match the lettered case histories/descriptions with
the numbered images 26-30.
A. Low-grade astrocytoma
B. The most common primary malignant brain tumor in adults.
C. Benign supratentorial extra-axial tumor.
D. Patient with unilateral hearing loss.
E. Bitemporal hemianopsia and Cushingoid features.
26 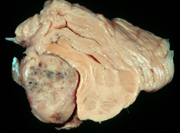 27
27 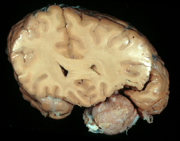 28
28 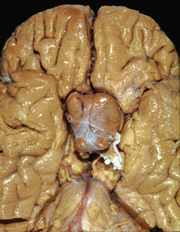 29
29 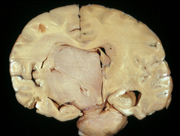 30
30 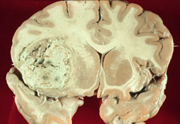
QUIZ 7 (same instructions as above, images 31-35)
A. 28-year-old trauma victim with a left subdural hematoma. After admission, patient developed a nonreactive, dilated left pupil.
B. Collapse and death moments after performance of a lumbar puncture in a patient with hydrocephalus.
C. 16-year-old gang member, deposited at emergency room dead. Examination revealed bitemporal skull defects and gross scalp hemorrhage.
D. Patient with alcoholic liver disease who fell, coming out of a bar, and hit his occiput.
E. 3 month-old baby admitted for lethargy following accidental fall. Radiograms reveal rib fractures of varying ages.
31  32
32 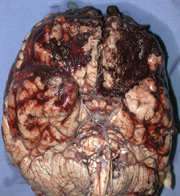 33
33 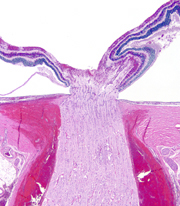 34
34 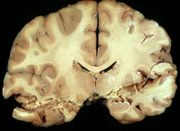 35
35 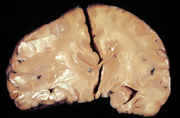
#33 is a longitudinal section of portion of the optic nerve and posterior part of the eye.
QUIZ 8 (same instructions as above, images 36-40)
A. Motor vehicle accident victim, unrestrained, without identifiable skull fracture.
B. Patient with left parietal GBM, temporal lobe herniation, and right homonymous hemianopsia.
C. Patient with severe headache. Arteriography reveals a ruptured MCA aneurysm.
D. Alcoholic patient with a history of fall and left subdural hematoma.
E. 6 year-old boy with acute lead poisoning, severe cerebral edema, and cerebellar tonsillar herniation.
36 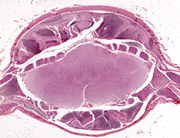 37
37 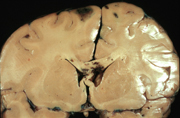 38
38 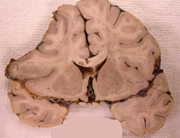 39
39 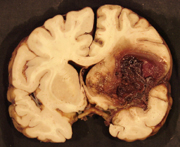 40
40 
QUIZ 9
Read case histories A through E. Write your
diagnoses below.
Case A
Case B
Case C
Case D
Case E
Match the case histories with images 41-45.
41 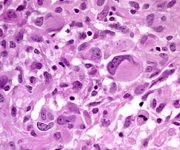 42
42 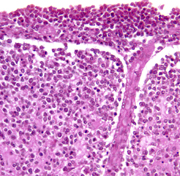 43
43 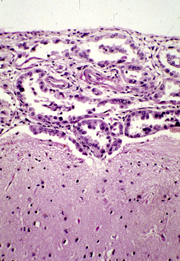 44
44 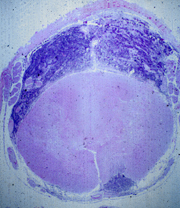 45
45 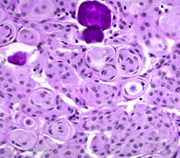
Case A
A 70-year-old man had a sudden onset of slurring of
speech and right arm weakness which resolved in 30
minutes. However, right hemiparesis, facial paralysis,
and slurred speech reappeared insidiously within
a few days and progressed. MRI revealed an enhancing
mass involving the left frontal lobe, basal ganglia,
and internal capsule. The patient had AIDS which
he had presumably acquired from a blood transfusion
several years earlier, in the course of partial gastrectomy
for peptic ulcer.
Case B
A 50-year-old man had seizures in the left hand for
several years. Then weakness of the hand and arm
developed, followed by a drop of the left side of
the mouth. Seizures became more frequent and headaches
appeared. Brain MRI revealed a right parasagittal
extra-axial mass which was totally resected, leading
to complete recovery.
Case C
A 74-year-old woman who had a right parietal headache
for one month developed weakness and numbness of
the left hand and began to drop things. The whole
left arm then became weak, and drooping of the left
side of the mouth developed, along with a sensation
of thick tongue. Weakness progressed to involve her
left leg, and a defect in the left visual field appeared.
MRI revealed an enhancing right parietal mass. A
craniotomy was done, and a necrotic tumor was partially
resected.
Case D
A 3 year-old girl had a cerebellar tumor which was
partially resected. She received intrathecal chemotherapy
and craniospinal irradiation and was stable for ten
months. Then, she developed tingling of the toes,
back pain, and weakness in the legs. A lumbar puncture
revealed tumor cells in the CSF. Symptoms progressed,
and within three months she lost sensation below
the chest, and became paraplegic and incontinent.
Additional chemotherapy and irradiation was given,
but she died four months later.
Case E
A 62-year-old woman who had had mastectomy for breast
cancer two years earlier gradually became confused,
ataxic, weak, and dysarthric. Head CT was normal.
CSF was clear with protein 136 mg/dl, glucose 14
mg/dl, and 30 lymphocytes. Her condition worsened,
and a succession of cranial nerve deficits appeared.
She deteriorated further, became comatose, and died
2 ½
months after the onset of the neurological symptoms.
QUIZ 10 (microscopic
pathology - same format as above)
Read case histories A through E. Write your diagnoses
below
Case A
Case B
Case C
Case D
Case E
Match your diagnoses with images 46-50.
46 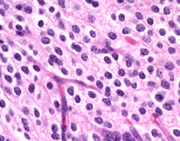 47
47 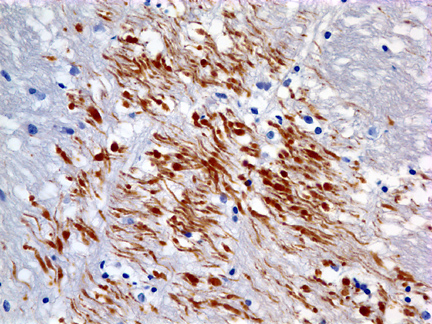 48
48 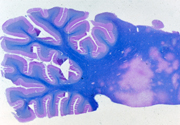 49
49 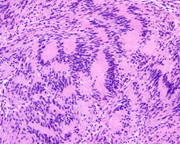 50
50
Case A
A 7 year old boy was an unrestrained passenger in
the front seat when the car in which he was riding
was hit by another car on the left side. The air
bag deployed, hitting him in the left temple. In
the ER, he was unconscious, responding only to painful
stimuli by extensor spasms. He had a scalp laceration
and fractures of the skull and left jaw. One week
after the accident, he was still unconscious. His
pupils and eye movements were normal, corneal and
gag reflexes were present, and he had no facial weakness.
He had weakness, spasticity and brisk tendon reflexes
on the right. Both plantar responses were extensor.
He lay most of the time with eyes open and had coordinated
eye movements following sounds and moving objects.
He appeared to sleep at times but could be roused.
He died of pneumonia and sepsis 10 days after the
accident.
Case B
A 4 year old boy had headaches and frequent vomiting
in the morning for 2 weeks. Examination by a pediatrician
and gastroenterology referral revealed no abnormalities.
The symptoms worsened. He became incoordinated and
his vision became blurred. Fundoscopic exam revealed
papilledema. MRI showed a cystic cerebellar mass.
A posterior fossa craniotomy was done and a partly
cystic lesion was removed.
Case C
A 39-year-old woman with Hodgkin’s disease developed
a rapid succession of neurologic deficits. First, there
was left facial weakness, followed by ataxia and weakness
of the left hand. One month later, a left visual field
cut appeared, then left hemiparesis. CSF was normal.
MRI showed areas of demyelination without mass effect.
Two months later, right hemiparesis and upward gaze
paralysis appeared. Gradually she became comatose and
died four months after the onset of her illness.
Case D
A 14 year old boy had buzzing in the left ear
and tingling and pain in the left face for one
year. Loss of hearing and vetigo gradually developed.
Neurological examination revealed weakness and
sensory loss on the left face. MRI revealed a
2.5 cm extra-axial mass in the left cerebellopontine
angle, extending into the left auditory meatus.
His mother had a spinal cord tumor removed when
she was 34 years old. The tumor was removed entirely
through a posterior fossa craniotomy.
Case E
A 61 year old man had a history of focal seizures
involving the left arm for 4 years. Gradually,
weakness and spasticity of the left arm and face
developed. Imaging studies reveiled an isodense
poorly defined, nonenhancing mass in the right
posterior frontal area, above the Sylvian fissure.
The lesion involved cortex and white matter.
Fine calcification was noted on the CT. A biopsy
was done.
NEUROPATH LAB - 3
QUIZ 11
QUIZ 12
QUIZ 13
QUIZ 14
QUIZ 15
For each projected numbered image 51-55, select the the single best description or diagnosis,
A. Bilirubin encephalopathy
B. Periventricular leukomalacia
C. Porencephaly
D. Multicystic encephalomalacia
E. Hydrancephaly
51  52
52  53
53 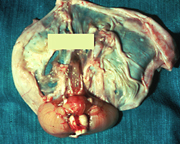 54
54 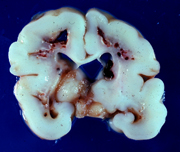 55
55 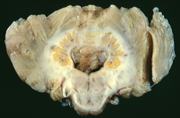
QUIZ 12 Same as above, images 56-60
A. 53 year-old man with a 1 year history of choreoatherosis, personality change, and dementia.
B. 67 year-old patient with recent onset of dementia, incontinence, and abnormal gait.
C. 47 year-old woman with remitting and exacerbating multifocal neurological deficits for 6 years.
D. 79 year-old patient with rigidity, bradykinesia, and tremor.
E. 76 year-old patient with a 6-year history of progressive memory loss, disorientation, and dementia.
56 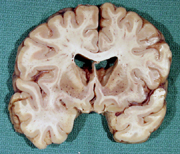 57
57  58
58 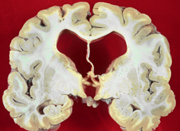 59
59  60
60 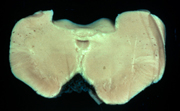
QUIZ 13
Same as above, images 61-65
A. Lifelong seizures and fatal intracerebral hemorrhage. Hemorrhagic CSF.
B. Diabetic coma, sinusitis and cerebral infarcts. CSF shows increased cells (polys and lymphs), elevated protein and low glucose.
C. Headache, fever, and stiff neck. CSF shows 850 neutrophils, increased protein, and low glucose.
D. History of IV drug abuse, low T4 lymphocytes, and dementia. Normal CSF.
E. Positive PPD, headache and cranial nerve deficits. CSF shows 89 lymphs, elevated protein and low glucose.
61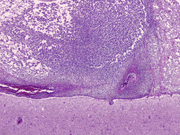 62
62 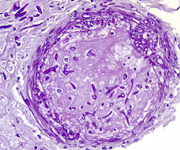 64
64 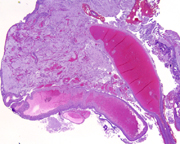 65
65 #63 is a PAS stain
QUIZ 14
Read case histories A through E. Write your
diagnoses below.
Case A
Case B
Case C
Case D
Case E
Match the case histories to images 66-70.
 67
67 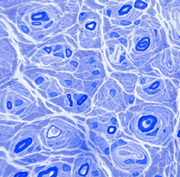 68
68 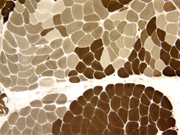 70
70 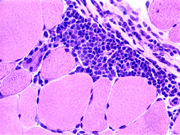
#67 is a thin plastic section of nerve stained with
toluidin blue.
#69 is a section of muscle with a histochemical-ATPase-stain.
Case A
A boy who was normal from birth through the first year of life, began to walk at 15 months and always had a waddling gait. He was never able to run as well as other children did. By the time he was 3 years old, he could not get up from the floor without pushing on his knees. At age 5, he could not climb stairs and began to walk on his toes. His calf muscles were bulky and felt rubbery. He was a slow learner at kindergarten. Serum CK was 2,735 (normal 3-35). His mother had a CK of 73. A muscle biopsy was done. A maternal uncle died of a similar disease at 15 years of age.
Case B
A 45-year-old woman had some clumsiness of the right
hand for three months. Her elbows, shoulders, knees,
and thighs ached. About four weeks following the
onset of these symptoms, she began to have difficulty
swallowing solid food. She fell easily, could not
climb stairs without supporting herself with her
hands, and could not get out of a low chair by herself.
Sensation was intact. CK was 887 (normal 3-35) and
sedimentation rate 42. A muscle biopsy was done.
Case C
Two weeks after having the flu, this pregnant (first
trimester) woman noted tingling of her hands and
weakness of the legs. The weakness progressed rapidly
and in 9 days she was bedridden, unable to move against
gravity or even shut her eyes. Initially, the diagnosis
of ‘hysterical reaction” was made, but
she developed difficulty breathing, had a tracheostomy,
and was put on a respirator. CSF was clear with glucose
81, protein 128, and 1 WBC. She had a cardiac arrest
and died four weeks after the onset of her illness.
She remained paralyzed until her death.
Case D
A 15-year-old boy had bilateral high arch feet, weakness
and atrophy of the legs and mild weakness of the
arms. He had no sensory loss or ataxia. CK was normal.
His grandfather, father, and uncle had a similar
condition.
Case E
A baby girl, one of twins, was 2 pounds 11 ounces
at birth. During pregnancy, no fetal movement was
felt by the mother until the eighth month. As a newborn,
she was hypotonic. She developed slowly, and, at
six months of age, she was unable to lift her head
or roll over. CK was normal. At 12 months, she was
extremely weak and hypotonic. Spontaneous movements
were apparent only in the hands and arms. Fasciculations
of the tongue were noted. Her twin brother and another
sibling died of a similar disease. Six other siblings
are normal.
QUIZ 15
Read case histories A through E. Write your
diagnoses below.
Case A
Case B
Case C
Case D
Case E
Match the case histories with Images 71-75. Each image
will be projected for one minute.
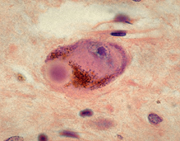 72
72 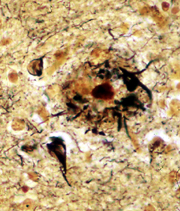 74
74 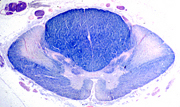 75
75 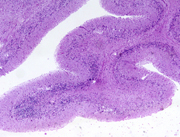
#74 is a myelin stain.
Case A
A 56-year-old woman developed paranoid ideas and difficulty
naming objects. She lost vocabulary, and her speech
became repetitive and stereotyped. She appeared anxious.
Memory failure developed (though she could remember
songs), and dementia set in. She became confused
and withdrawn and began to perform ritualistic tasks.
She had no seizures or motor deficits. Dementia progressed,
and she died in a nursing home 7 years after the
onset of her disease.
Case B
A 62-year-old man had tremor of the hands and head
and rhythmic tongue protrusion. He became stiff and
walked with small steps in a stooped posture. He
was treated with L-dopa and other medications without
significant improvement. Four years after the onset
of these symptoms, intellectual deterioration and
memory loss developed. He died in a nursing home
at age 69.
Case C
A 58-year-old woman had a gradual onset of difficulty
walking characterized by staggering, especially when
walking in the dark. She had no history of alcoholism
and was well nourished. Neurological exam revealed
a wide-based gait and abnormal cerebellar testing.
While gait difficulty progressed, tremor of the hands
and difficulty writing appeared. She had a mask-like
face. Treatment with sinemet was without effect.
Then, she developed orthostatic hypotension and bladder
incontinence. Mental status remained normal. She
died 14 years after the onset of her illness.
Case D
A 70-year-old man developed progressive confusion,
difficulty sleeping, and jerks of all limbs. The
symptoms worsened and he lost fine motor control
of both hands and became ataxic. He became confused
and demented. Speech was an incomprehensible jargon.
CSF was normal. MRI revealed mild cortical atrophy.
EEG was abnormal. He died four months after the onset
of his illness.
Case E
A 63-year-old man developed weakness of the left leg
and then of the right leg and both hands. His grip
became weak and he began dropping things. Weakness
progressed, resulting in frequent falls. His voice
changed and he began to drool and had difficulty
swallowing. He became bedridden. There were fasciculations
of his tongue. Deep tendon reflexes were hyperactive,
and plantar responses were extensor. Intelligence
and sensation were not affected. He had difficulty
breathing and died three years after the onset of
his illness.