EXPERIMENTAL ALLERGIC ENCEPHALOMYELITIS
Experimental allergic encephalomyelitis (EAE) has been used for years as an experimental model of MS. It can be induced in mice, rats and guinea pigs by intradermal injection of whole CNS tissue or myelin basic protein (MBP). Two weeks after the injection, the experimental animals develop ascending paralysis. The injection of MBP triggers a cell-mediated immune reaction against the recipient's myelin. MBP-specific T-cells traverse brain capillaries. Interaction of these cells with MBP activates them and results in secretion of cytokines, damage of the blood-brain barrier, and recruitment of macrophages. Microscopic examination shows perivenular lymphocytes, similar to acute MS, but little or no demyelination. EAE can be induced by injection of MBP-specific T-cells. Classic EAE is a monophasic reaction. A chronic relapsing EAE has been induced in guinea pigs. EAE can also be induced by other myelin proteins that are chemically different from MBP, and by nonmyelin proteins such as S100 protein. Injection of MOG (myelin oligodendrocyte glycoprotein) along with transfer of anti-MOG lymphocytes can cause demyelination. While EAE proves that an autoimmune reaction can cause inflammation in the white matter, the analogy with MS stops there. The immunology and pathology of MS are far more complex than EAE.
ACUTE DISSEMINATED ENCEPHALOMYELITIS
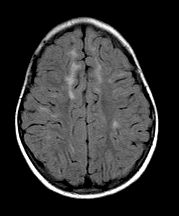
Acute disseminated encephalomyelitis (ADEM), also known as postinfectious, postvaccinal, or allergic encephalomyelitis, is an acute demyelinating disease, which most commonly affects children. It develops usually a few days to four weeks following a nonspecific upper respiratory infection or after infection with a variety of other viral and bacterial agents, including Epstein-Barr virus, cytomegalovirus, or mycoplasma pneumoniae, and following vaccinations. Sometimes it appears without a preceding infection. After an initial phase characterized by malaise, fever, headache, stiff neck, and drowsiness, encephalopathy (mental status change, psychiatric manifestations) and multifocal deficits (hemiplegia, ataxia, sensory abnormalities, visual loss) appear within hours or a few days. Ataxia is especially common in ADEM following varicella. The MRI shows multiple, bilateral, asymmetric, hyperintense lesions with fuzzy margins (as opposed to the sharp demarcation of MS plaques) in the subcortical and deep white matter, deep nuclei, cerebellum, brainstem, and spinal cord. Some large confluent lesions resemble brain tumors because of perilesional edema and mass effect. The CSF may be normal or show mild lymphocytic pleocytosis and increased protein. There are no oligoclonal bands.
Most ADEM cases are monophasic and self-limiting, and have a favorable outcome, especially after treatment with high dose IV corticosteroids. However, rare cases are severe or even fatal and a few cause permanent neurologic deficits. Typically, the clinical course of ADEM evolves over a period of 3 months and the MRI abnormalities resolve after that time. New symptoms or MRI abnormalities after 3 months may represent multiphasic ADEM, which is rare, or transition from ADEM to MS, optic neuritis, or neuromyelitis optica.
Pathologically, ADEM is characterized by perivenous sleeves of inflammation (mainly T- lymphocytes and macrophages), edema, demyelination, and axonal loss. The lesions are all of the same age and affect white matter and gray matter, including cerebral cortex and deep nuclei. There is microglial activation in the cortex. Acute hemorrhagic leukoencephalitis (Weston-Hurst syndrome) is a fulminant, frequently fatal form of ADEM with extensive, confluent white matter lesions, characterized by vascular necrosis, acute inflammation, hemorrhage, and edema.
ADEM is not an infection. It is thought to be a T-cell mediated immune reaction triggered by the preceding viral infection or vaccination. Similarity between viral and myelin proteins probably accounts for some ADEM cases. In this scenario, sensitized T-cells attack not only the pathogen but also neural tissues that contain similar proteins. Rabies vaccines prepared from brains of inoculated sheep are contaminated with CNS tissue. ADEM following such vaccination is analogous to EAE. It is due to sensitization against myelin antigens that are present in the vaccine. Alternatively, CNS tissue and vascular damage that occur in the course of some infections exposes CNS (myelin) antigens to the immune system. Autoreactive T-cells, generated in this process invade the brain and destroy myelin.
ADEM should be distinguished from acute necrotizing encephalopathy (ANE), a parainfectious condition that appears following febrile viral infections such as influenza and parainfluenza. ANE is characterized by symmetrical involvement of the thalami and other structures. Some ANE cases, referred to as ANE1, are genetic autosomal dominant, and are caused by mutations of RANBP2 (on chromosome 2q11-13).
Further Reading
- Tenembaum S, Chitnis T, Ness J, et al. Acute disseminated encephalomyelitis. Neurology 2007;68(Suppl 2):S23-S36 PubMed
- Pohl D, Alper G, Haren KV, et al. Acute disseminated encephalomyelitis. Updates on an inflammatory CNS syndrome. Neurology 2016;87 (Suppl 2):S38–S45. PubMed
- Singh RR, Sedani S, Lim M, et al. RANBP2 mutation and acute necrotizing encephalopathy: 2 cases and a literature review of the expanding clinico-radiological phenotype. Eur J Paediatr Neurol 2015;19:106-113.PubMed
Updated: October, 2017